I was first diagnosed with ILD (Interstitial Lung Disease) or IPF (Idiopathic Pulmonary Fibrosis), as the condition is more widely known, in June 2016. My symptoms were shortness of breath and dry coughing. As my condition worsened, I was put on supplementary oxygen after my first exacerbation in December2016. Since then, my health rapidly deteriorated and I was left with no other option but to undergo a lung transplant. After a detailed evaluation, it was decided that I needed a double lung transplant and, on October 21, 2017, I had my transplant.
Life after my lung transplant has been nothing short of a blessing. I am leading an extremely normal life and am able to breathe freely on my own, which wasn’t possible during the progression of my condition. I am able to go to work on a regular basis and I can also undertake regular activities in my day to day routine life. I have also traveled abroad twice (Dubai in August 2018 and South Africa in May 2019) apart from the trips that I have undertaken within India without any sort of hindrance or discomfort. I would also like to request everyone to come forward and become aware about organ donation which can go a long way in saving lives. – Tushar Kataria, Mumbai.

Tushar is one of my patients and is doing well. If you, or someone you know, have been told that you/they need a lung transplant, or you are wondering if a lung transplant may be helpful, then it would be useful to familiarize yourself with some important aspects of lung transplantation.
What is a lung transplant?
It is the replacement of a patient’s lung or lungs with lung from a donor, and hence it involves removal of the patient’s lungs and implanting the donor lungs. It is used body if it is deemed that the patient’s own lungs are in end stage organ failure.
What is the meaning of end stage lung failure?
The normal function of lungs is to get air from outside (inhalation) and expelling air back outside (exhalation). This is called the ventilatory function, and is dependent on normal functioning of the brain, spinal cord, muscles of the chest, abdomen and neck, the rib cage, as well as the lungs themselves. This means that this function can be affected by diseases that do not necessarily affect the lungs directly.
The other major function is the gas exchange function (which is the ability to take in as much oxygen as needed by the body and expelling the carbon dioxide produced by the cells). This is done at the interface between the air sac (alveolus) and the blood vessels in the lung (capillaries), hence it is called alveolar capillary membrane. Diseases that damage this area can lead to an inability to take in oxygen (type 1 lung failure) or, additionally, to an inability of expelling carbon dioxide (type 2 lung failure).
An irreversible failure of the gas exchange function that is progressive is called end stage lung failure. It occurs commonly when there is scarring of the lung tissue (fibrosis) or damage from smoking (emphysema). It can also occur from diseases affecting the blood vessels to the lung (pulmonary hypertension).
Does everyone with end stage lung failure need a lung transplant?
No, transplantation is a procedure that has its own limitations and complications. Only when doctors have fully assessed the situation and decided that medicines are not of use and the benefit from a lung transplant will outweigh the risk, is a transplant recommended.
I have been told by my doctors that I need a transplant. Do I just need to register and wait?
The first step is to have a full evaluation by the team that is going to do the transplant. This evaluation will see if indeed no other therapy is possible, it will determine the current state of the disease (how long can you wait without a lung transplant), and finally it will also determine if there are any reasons why a transplant cannot be done. If you are an eligible candidate, then registration according to the rules in your state can be done.
Why would I be ineligible for a transplant, even if I need one?
If there is a recent diagnosis of cancer, or evidence of an active infection, then that may rule out a transplant. However,if the patient has some problems like uncontrolled diabetes, hypertension, being very frail, or evidence of damage to other organs, this can be worked on by a dedicated team and improved. Once that is done, the patient can be listed for a transplant when the risk of transplant surgery improves.
What will be the important things for the patient to do while awaiting a lung transplant?
The disease process at work in patients awaiting a lung transplant and medicines like steroids that are being used will make them very weak. This may make it difficult for them to breathe by themselves even if the lungs are working well. Healthy nutritional intake, supervised exercise and pulmonary rehabilitation are very important to reduce the risk from the operation.
What happens during the operation?
When an eligible donor becomes available (this can happen at any time and you should be ready 24/7), you will be alerted and should reach the hospital where your surgery will take place. A donor assessment team will ensure that the donor lung has good function and the donor does not have any diseases that can be transmitted to the patient. If that is okay, then the operation usually commences simultaneously. This means that the retrieval of lungs from the donor happens at the same time as the removal of diseased lungs from the recipient. This is done so that the organs can be implanted immediately on arrival so that the time duration that the organ is deprived of blood (ischemic time) is as short as possible.
How many kinds of lung transplant are there?
Depending on your condition, you could be advised a single lung transplant (only one lung, the right or the left, could be transplanted), or a double lung transplant (both lungs will be transplanted). In some situations, when the disease has severely affected both heart and lungs, a combined heart and lung transplant is done. Each one has their own set of advantages and disadvantages.
What to expect in the period after the lung transplant?
In the period immediately after the transplant, you will be in the intensive care unit on a breathing machine. Once able to breathe on your own, you will be taken off the breathing machine. The next few days you will have intensive monitoring for infection, rejection and any other complications that may occur. If well, you will be discharged home with some nursing help in anywhere between 14-21days.
The first month will require visits with your doctor to ensure that food, physiotherapy and medicines are all being done correctly. A routine biopsy to look for rejection may or may not be done according to the protocol in your hospital.
The next year will require follow up and, perhaps,a decrease in medicines required if you progress without any complications. You will require periodic follow up with less frequency after the first year.
What are the main problems associated with lung transplants?
Lungs tend to encounter more rejection than other organs like kidney, heart or liver. In addition, the risk of infection is higher as they are constantly exposed to the environment. Rejection could be acute (usually happening after days to weeks or months after surgery) or chronic (over months or years). In general, the incidence of serious infection and episodes of acute rejection go down significantly in frequency after the first year, but surveillance will need to be maintained.
Is it okay to have a lung transplant in the current COVID pandemic?
As the pandemic has been unfolding over the last 5-6months, it will not be possible to accurately predict the general risk of having a lung transplant during the pandemic. However, as the lung is the primary portal of entry and alsothe target of the virus, caution is required. The Tamil Nadu Transplant Authority (TRANSTAN) and National Organ & Tissue Transplant Organization (NOTTO) have issued guidelines for safe conduct of transplants. These include ensuring the donor and recipient are COVID negative, the tests being done as close as possible to the time of surgery. There are also guidelines for the maintenance of a dedicated team for the lung transplants that is routinely tested.
Is lung transplant a treatment for COVID-19?
There are a few isolated examples from China and one from the US. The short-term (surviving outside hospital) outcomes are unclear. In any case, in patients who have survived the initial attack on the lungs but suffer from severe lung damage (fibrosis), it has to be determined that they are no longer actively infective before consideration. This will be a very small number of eligible patients, and by no means can lung transplant be considered a cure for COVID.
Can you describe the quality of life after a lung transplant?
This question is best answered by the persons who have undergone the experience as no one else can ever hope to understand what it feels like. So below is life before and after transplant in their own words.
Jitendra Thadeshwar, Mumbai.
I had a double lung transplant on the 27th of March 2018. Before I got operated, I was on 2 to 3 liters of oxygen 24/7 and mostly in bed. Used to suffer from back pain too, which got completely sorted after the operation.
Got up in the ICU. The respirator was out and on 2 liters of oxygen by day 2, was sitting in a chair by day 3. In the regular ward on day 4, by then the oxygen was reduced to 1 liter which I wanted to keep (old habits die hard). The doctors suggested to get rid of the oxygen as I didn’t actually need it, and with a lot of hesitation I did. Had started doing physio, and by day 6 most of the pipes were out of my body and was walking in the corridor and even climbed steps. Left the hospital with a male nurse on day 8.
Each day after that was a better day, though painful at times, but much better. Luckily in my case the walking and physio went really smooth, maybe because I was an avid trekker all my life. After one bronchoscopy a month later, I did not require any. By May I was back in Mumbai.
After 6 months of the surgery, life was mostly back to normal. I was doing all my daily chores without any problems and was most excited to get back to driving my car again. Went for a few long drives – self-driven. Resumed work by 9th month, went for my first international holiday a year later. Followed by a few holidays in India. It has been more than 2 years now. Before the Covid situation happened, I was walking 5 km every day, followed by gymming and normal day to day activities, considering the only wish I had post operation was to achieve a normal shower and decent meal everyday
Jitendra Pre-Transplant

Jitendra Post-Transplant

Rajasekar, Chennai
I developed breathing difficulties while performing regular physical exercises. I was diagnosed with Interstitial lung disease (ILD). I had my double lung transplant in July 2017. I was discharged from the hospital in ten days. At the time of discharge, I was given in depth advice on do’s and don’ts, diet, physical fitness patterns, cleanliness etc. which helped me a lot during the recuperation period over the next six months. Before 2015, my weight was 60 kg, which came down to 41 kg before the day of surgery. Now I have fully recovered, and my weight is 66 kg. Six months after the operation, I started attending office. I am now enjoying my new lease of life and attending to my home and office chores as usual without any difficulty. I also got married a few months ago.
Ravi, Chennai
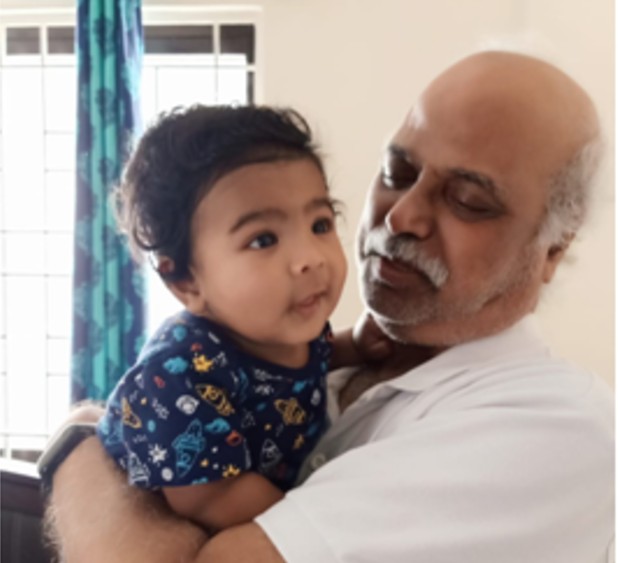
Life after lung transplant is slow recovery. Once recovery takes place, it feels like one has new lease of life. Above all, have a positive attitude, live your life and, as far as possible, reduce stress issues and take more rest. I have taken a few pictures of myself. I think a picture speaks a thousand words.
Ravi Post-Transplant

Yanamandra Satya Prasad, Karnataka
After a double lung transplant in January 2018, I am leading an almost normal life. Life after a double lung transplant is extremely beautiful when compared to that prior to my operation. I cannot think about big and portable oxygen concentrators I was using and was almost confined to my house.
Puspha, Bengaluru.
I was diagnosed with PPH (primary pulmonary hypertension) in 2011. I was on medication for a few years and everything was going on. After few years, I became sick, and my sister and I went to Chennai in 2014. I was asked to take a few medications and to use oxygen(2L). Later in 2017, doctors suggested to undergo “heart and a double lung transplant”since my condition was worsening. We waited to get a donor of perfect size of mine. We waited for one year two months. Once the surgery was done, I was little down for few days, which was really painful for me, and I was coping with it. There was a full-time nurse to guide me in everyday activities, and they gave me a lot of support. By god’s grace I am doing good and came back to my hometown after two months of my surgery. I am really happy now that I am back with my family and my friends. I am feeling active and healthy now after my surgery.


You and your team are doing an incredible job, Dr Paul Ramesh. I’ve had the privilege of seeing first-hand the dedication and care you bestow upon these very sick patients…patients who thanks to your efforts are now back to a normal life.
Keep up the good work, God bless you and your team!
Raj
You are doing good job. After the long procedure of the surgery patient take new birth and the date of transplant his /her 2nd birthday. I think patient should be Celebrate it with his doc and family. Its owsome and GOD give you lots of power to the Doc. Lots of blessing for you and your family who support and give you more energy to do this kind of work and Help the patients.
Thanks and Regards
Pramod Saini